NEWS2 score for assessing the patient at risk of deterioration
2019
The RCGP supports the use of physiological measurements in a general practice setting for all patients at risk of deterioration.
More research evidence on the use of NEWS2 in a primary care setting is required. Only then can the RCGP consider recommending its widespread uptake in general practice.
Sudden acute deterioration in health can occur as a result of a wide variety of causes across all systems. This includes infection, cardiovascular issues, haemorrhage and embolism amongst others. These high-consequence pathological conditions can present in the community. It is important that they are recognised and managed appropriately in general practice.
The unwell patient at risk of deterioration presenting in general practice requires the clinician to:
- Identify relatively unusual but well recognised acute presentations
- Assess the patient appropriately
- Respond and provide interventions (where appropriate) to start treatment or stabilise the patient
- Effectively communicate their assessment to achieve a timely response from colleagues within the healthcare system. This includes, for example, ambulance switchboard, paramedic and secondary care teams.
NHS England have recommended the National Early Warning Score (NEWS2) as a universal scoring system. This is for use across the NHS within ambulance and secondary care services for the patient at risk of deterioration. It is in order to standardise practice, stratify risk, and aid communication between services. This was communicated as a Patient Safety Alert and was implemented in March 2019. It did not mandate its use within general practice. However, it noted that work was taking place to identify evidence within the community and primary care. There are calls for GPs to use NEWS2 scores as part of their clinical assessment of acutely deteriorating patients. This particularly applies to those requiring inpatient care and ambulance transportation.
Clinical policy
Assessment of physiology has always been part of medical practice and aids clinical judgement when assessing patients, with changes in physiology helping to determine if a patient is improving or getting worse. The relative importance and predictive value of abnormal physiology in identifying gradual deterioration and stratifying risk at presentation has been studied for over a decade.5-7 Physiological assessments can either be used as single parameters to predict deterioration, for example, through the use of “Red Flag” systems8,9, or can be combined and weighted, to form a predictive risk tool, such as NEWS2. The predictive value of the Red Flag systems in hospital and ambulance settings are inferior in both sensitivity and specificity.10,11
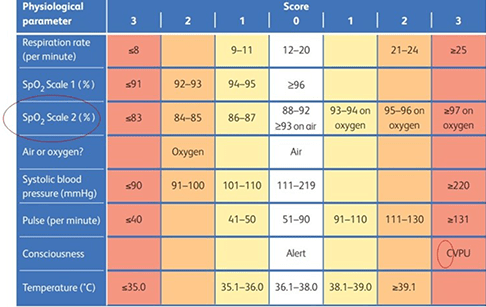
The Royal College of Physicians launched NEWS scoring system for non-pregnant adults aged 16 or over, in 201212. Physiological measurements (including respiratory rate, oxygen saturations, temperature, systolic blood pressure, pulse rate and level of consciousness) are taken and given a score. The aggregated score has been validated within hospital and ambulance settings as an adjunct to patient assessment by clinical and non-clinical staff. It can be used to assess if the patient is at risk of dying or requiring admission to intensive care. It is used as a tool to escalate concern to more senior clinicians and/or mandate urgent actions. The tool was updated December 2017, creating NEWS21, which added an additional oximetry scale for assessing those with chronic hypoxia, confusion of acute onset in the assessment of mental function, and the range of the physiological parameters within Table 1.
NHS England has adopted the use of NEWS2 in all secondary care and ambulance services since 2019, implementing NEWS2 as their common language for communicating concern regarding deteriorating patients. It has been proposed that all patients aged 16 and over, who are not pregnant requiring a level 2 emergency ambulance, are, wherever possible, to have their vital signs measured (pulse oximetry, blood pressure, respiratory rate, temperature, pulse rate and conscious level), and handed to the operator at time of ambulance dispatch. NHS England asks that if possible, a NEWS2 score is also calculated and handed over to paramedics upon arrival.4
There has been much discussion and debate between NHS England, the Devolved Nations health administrations, secondary care, the British Medical Association and the RCGP regarding the implementation of NEWS2 scoring in a general practice setting. It is not recommended as a replacement for clinical judgement but as an adjunct to patient assessment and a tool to help convey concern. Currently, assessment as to whether a patient is deteriorating is a clinical judgement supplemented by the recording of some physiological values and single parameter assessments. Some areas of the country are using NEWS2 to assess all parameters and augment the GP clinical judgement, but not as a replacement for the judgement. Typically, where this is happening it is subject to careful governance and evaluation.
NEWS2 in Ambulance Services, Emergency Departments and Secondary Care
NHS England has now adopted the use of NEWS2 as the preferred scoring system to use when tracking potential patient deterioration to ensure a single universal language is used.26
NEWS2 has been validated in secondary care showing it has the best sensitivity and specificity of all the early warning scores1. Early warning scores have been found to be strong predictors of adverse outcomes13-20 and an association has been shown between mortality and elevated initial early warning scores at first presentation to secondary care8,17, emergency departments18 and ambulance services19-21. Early warning scores have also been shown to have a higher predictive value than single parameter scoring systems, including “Red Flag” systems often used in primary care8-10.
Current practice in primary care
Typically, general practice makes decisions using clinical judgements drawing on patient history and a single point set of physiological measurements. The NCEPOD ‘Just Say Sepsis’22 noted that there was poor recording of physiology of patients at the appointment prior to hospital admission with sepsis, and the RCGP Sepsis Spotlight Survey 201723 also identified a lack of routine use of physiological measurements in primary care in this group. Furthermore, physiological measurements known to have the least predictive value in secondary care settings for the identification of sepsis, (temperature, pulse and oximetry), were more likely to be recorded in these primary care studies23,25, and conversely, the most predictive physiological measurements for identification of sepsis, (respiratory rate, cognition and blood pressure), were the least commonly recorded.
NEWS2 in primary care
NEWS2 has not been validated in general practice yet. There is limited evidence on its use demonstrating that NEWS2 can be delivered in general practice at scale,27,28. An unpublished primary care study by the Wessex Academic Health Sciences has found an association between 30-day mortality and NEWS2 values, with mortality increasing rapidly with scores of 5 or above. This is similar to the association between elevated NEWS2 score and mortality in patients referred from other locations. However, no data is yet available to determine if this improves clinical outcomes or ensures appropriate and timely admission for the right patients.
The use of NEWS2 in primary care offers a potential benefit in improving communication between GPs, ambulance services and secondary care services by using the same “common language” that the ambulance trusts have been mandated to use since 2018, It also has the potential to improve GP to GP communication when patients re-present to different GPs or different services for further assessment, enabling deterioration to be identified objectively, in addition to clinical judgement and single point measurement of physiological parameters.
There are, however, equipment and possible financial barriers to the fullest implementation of NEWS2 in general practice, including access to calibrated equipment. Pulse oximetry will need to be universally available - simple digital devices can be used but will not suitable for all patients and may need to be upgraded include earlobe oximetry25 (useful when poor peripheral perfusion or plastic nails present an issue). An upgrade of the equipment generally available in general practice will be required, with typical costs of approximately £600 per device. All other physiological measurements required for NEWS2 can be undertaken with equipment readily available in general practice.
From 2019, it has been proposed that all patients aged 16 and over who are not pregnant requiring a level 2 emergency ambulance, are, wherever possible, to have their vital signs measured and handed to the operator at time of ambulance dispatch. NHS England also ask if possible for a NEWS2 score to be calculated and handed over to paramedics upon arrival.4
NEWS2 is not yet validated in primary care and although unpublished data suggests it may be useful to predict 30-day mortality in acutely unwell patients. This work and other studies into GP use of NEWS2 are awaiting publication in peer reviewed journals.
- The RCGP recommends the use of physiological measurements when assessing patients at risk of deterioration in primary care
- The RCGP recommends that on requesting a level 2 emergency ambulance dispatch for patients (16 and over who are not pregnant), clinicians should, when possible, provide appropriate physiological measurements to the ambulance switchboard operator and paramedics upon arrival
- The RCGP does not recommend the use of NEWS2 as a replacement for clinical judgement
- The RCGP recognises that some areas and GPs currently use NEWS2 when assessing their patients and arranging their admission. This should be viewed as optional and ideally should be done as part of a governed system where its value to patient safety and care is being assessed
- The RCGP recommends further research on the use of NEWS2 in General Practice to validate its use in this setting.
- Royal College of Physicians. National Early Warning Score (NEWS) 2: Standardising the assessment of acute-illness severity in the NHS. In: RCP, editor. London: RCP; 2017.
- NHS improvement, resources to support the safe adoption of the revised National Early Warning Score (NEWS2). In: NHS Improvement, editor.; 2018.
- NHS England. NEWS frequently asked questions. 2018.
- Association of Ambulance Chief Executives. National Framework for Healthcare Professional Ambulance Responses. In: AACE, editor.; 2019.
- Subbe CP, Kruger M, Rutherford P, Gemmel L. Validation of a modified Early Warning Score in medical admissions. QJM 2001; 94(10): 521-6.
- Ridley S. The recognition and early management of critical illness. Ann R Coll Surg Engl 2005; 87(5): 315-22.
- Subbe CP, Slater A, Menon D, Gemmell L. Validation of physiological scoring systems in the accident and emergency department. Emergency medicine journal : EMJ 2006; 23(11): 841-5.
- Smith GB, Prytherch DR, Schmidt PE, Featherstone PI, Higgins B. A review, and performance evaluation, of single-parameter "track and trigger" systems. Resuscitation 2008; 79(1): 11-21.
- Tirkkonen J, Olkkola KT, Huhtala H, Tenhunen J, Hoppu S. Medical emergency team activation: performance of conventional dichotomised criteria versus national early warning score. Acta Anesthesiology Scand 2014; 58(4): 411-9.
- Kopczynska M, Sharif B, Cleaver S, et al. Red-flag sepsis and SOFA identifies different patient population at risk of sepsis-related deaths on the general ward. Medicine (Baltimore) 2018; 97(49): e13238.
- Camm CF, Hayward G, Elias TCN, et al. Sepsis recognition tools in acute ambulatory care: associations with process of care and clinical outcomes in a service evaluation of an Emergency Multidisciplinary Unit in Oxfordshire. BMJ open 2018; 8(4): e020497.
- Royal College of Physicians. National Early Warning Score (NEWS) Standardising the assessment of acute-illness severity in the NHS. RCP, 2012.
- Cattermole GN, Mak SK, Liow CH, et al. Derivation of a prognostic score for identifying critically ill patients in an emergency department resuscitation room. Resuscitation 2009; 80(9): 1000-5.
- Prytherch DR, Smith GB, Schmidt PE, Featherstone PI. ViEWS-Towards a national early warning score for detecting adult inpatient deterioration. Resuscitation 2010; 81(8): 932-7.
- Smith T, Den Hartog D, Moerman T, Patka P, Van Lieshout EM, Schep NW. Accuracy of an expanded early warning score for patients in general and trauma surgery wards. The British journal of surgery 2012; 99(2): 192-7.
- Corfield AR, Lees F, Zealley I, et al. Utility of a single early warning score in patients with sepsis in the emergency department. Emergency medicine journal: EMJ 2013.
- Smith GB, Prytherch DR, Meredith P, Schmidt PE, Featherstone PI. The ability of the National Early Warning Score (NEWS) to discriminate patients at risk of early cardiac arrest, unanticipated intensive care unit admission, and death. Resuscitation 2013; 84(4): 465-70.
- Corfield AR, Lees F, Zealley I, et al. Utility of a single early warning score in patients with sepsis in the emergency department. Emergency medicine journal: EMJ 2014; 31(6): 482-7.
- Silcock DJ, Corfield AR, Gowens PA, Rooney KD. Validation of the National Early Warning Score in the prehospital setting. Resuscitation 2015; 89: 31-5.
- Williams TA, Tohira H, Finn J, Perkins GD, Ho KM. The ability of early warning scores (EWS) to detect critical illness in the prehospital setting: A systematic review. Resuscitation 2016; 102: 35-43.
- Abbott TEF, Cron N, Vaid N, IP D, Torrance HDT, Emmanuel J. Pre-hospital National Early Warning Score (NEWS) is associated with in-hospital mortality and critical care unit admission: A cohort study. Ann Med Surg (Lond) 2018; 27: 17-21.
- NCEPOD. Just Say Sepsis. In: National Confidential Enquiry into Patient Outcomes and Death, editor. London: NCEPOD; 2015.
- Stockley S. RCGP Sepsis Toolkit. 2018.
- Seymour CW, Liu VX, Iwashyna TJ, et al. Assessment of Clinical Criteria for Sepsis: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). Jama 2016; 315(8): 762-74.
- NHS improvement. Risk of harm from inappropriate placement of pulse oximeter probes. 2018 (accessed 11/6/19 2019).
Thank you for your feedback. Your response will help improve this page.