Advice and guidance (A&G)
Updated April 2025
From 1 April 2025, NHS England have introduced the formal General Practice Requests for Advice and Guidance Enhanced Service (A&G ES), as part of wider changes to the national 2025/26 GP Contract in England. Backed by up to £80 million in funding, the ES encourages GPs to seek specialist advice pre-referral, with a £20 Item of Service (IoS) payment for each request to recognise the additional workload created for general practice. The RCGP welcomes this step, while emphasising the need for appropriate resourcing and investment in general practice to deliver A&G consistently across the country to support timely, safe, and appropriate care of our patients close to home.
The RCGP and BMA have worked with NHSE/I on guidance relating to the Advice and Guidance initiative, with direct access to investigations, to produce specialist advice clinical responsibility FAQs and specialist advice Medico-legal FAQs.
Further specifics of the service
Advice and Guidance (A&G) is a non-face-to-face, GP-led enhanced service within England that supports general practice teams to seek specialist advice from secondary care before, or instead of making a referral. It enables clinical dialogue between GPs and consultants to support non-urgent patient care, particularly in cases of diagnostic uncertainty or where referral thresholds may not be met. The types of advice that may be requested include, but are not limited to, treatment plans, interpretation of results and/or advice on appropriateness of referrals/tests.
Joint guidance on the NHS e-Referral Service (e-RS) developed by GPC England, NHS England, and NHS Digital notes that when properly implemented, the e-RS A&G feature ‘allows a multi-way conversation to take place between GPs and Consultants that can help strengthen professional relationships, share knowledge and promote important clinician-to-clinician dialogue around patient care’.
The government aims to increase pre-referral advice requests from GPs to up to four million in 2025/26 (up from 2.4 million in 2023/24) as part of wider efforts to cut waiting lists and improve patient care.
- All GP practices – whether operating under a GMS contract, PMS agreement or APMS contract – are eligible to opt in to the enhanced service, provided they meet the specified requirements. In 2022, the RCGP recommended that A&G should be optional and not mandated, and we are glad to see that participation is voluntary on an opt-in basis.
- A&G can be delivered in real-time/synchronously (e.g. telephone) or asynchronously (e.g. NHS e-Referral Service (e-RS) or secure email).
- A&G requests can be non-specific, they are not a prerequisite to formal referral, and do not start a referral-to-treatment (RTT) clock.
- Practices can claim a £20 Item of Service (IoS) payment for each GP-led pre-referral A&G request, including all related follow-up activity within a single episode.
- At a local level, Integrated Care Boards (ICBs) may introduce caps on claimable A&G activity per practice, to stay within the national £80 million budget for 2025/26. Practices can submit additional requests beyond the cap, but they will not be reimbursed.
Full details can be found within NHS England’s Enhanced Service Specification for General Practice Requests for Advice and Guidance 2025/26.
Our latest press responses
- ‘Funding must follow the patient’, College welcomes support for Advice and Guidance services (published 17 April 2025)
- Funding A&G services ‘a good step’ – RCGP responds to elective care plan (published 06 January 2025)
Updated May 2022
NHS Digital states that NHS e referral service (e-RS) advice and guidance (A&G) “is a two-way dialogue channel in the e-RS which allows GPs/referrers to seek specialist input into a patient’s care” providing “a secure rapid digital communication channel between two clinicians, the ‘requesting’ clinician and the provider of a service (the ‘responding’ clinician), enabling a patient’s care to be managed in the most appropriate setting”.
NHS Digital states that there “may be a number of reasons why a clinician may wish to use the service including:
- asking another clinician or specialist for their advice on a treatment plan and/or the ongoing management of a patient
- clarification (or advice) regarding a patient’s test results
- seeking advice on the appropriateness of a referral for their patient (e.g. whether to refer, or what the most appropriate alternative care pathway might be)
- identifying the most clinically appropriate service to refer a patient in to”
Since February 2021 the E-RS advice and guidance was amended, aiming to “reduce the burden on GPs/referrers”, by allowing “advice and guidance to be used as a referral channel”, thus preventing information passing back and forward between the requesting and responding clinician aiming to “streamline patient care”.
As a result of the pandemic and the backlog of care, there are now over 6.1 million people waiting for treatment after referral in England. Published data from February 2022 shows record numbers of people waiting, with over 2 million waiting longer than 18 weeks and 300,000 waiting longer than 1 year for treatment and the average waiting time being 13.1 weeks. At the same time, the number of primary care referrals to secondary care that were rejected, increased by 87% (from 238,859 in February 2020 before the pandemic began, to 401115 in November 2021).
When GP referrals are delayed or rejected, patient care does not end. These people and their carers are held in the community, cared for by primary care. This is increasing the workload pressure within the community and creating a backlog of care in general practice.
The RCGP understand that advice and guidance is being used by some providers to manage their waiting lists, (such as converting requests to referral to advice and guidance or using advice and guidance to decline referrals) which in some areas, is adding increased workload burden to primary care.
A recent survey (April 2022) of RCGP clinical advisers showed that almost all GPs (91.7%) used advice and guidance, with the vast majority (83%) finding it useful. Examples were given of rapid responses to questions that were helpful in streamlining patient care. The response times and quality of responses varied depending upon the individual clinician, specialty and geography; with some respondents stating that there were unacceptable delays in gaining answers to questions necessitating increased holding of risk and patient care delays within primary care.
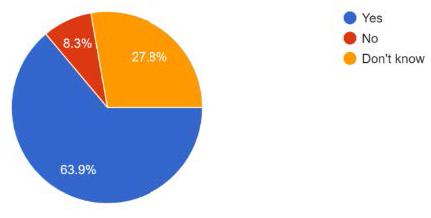
64% of respondents believe that the advice and guidance was being used as a referral management tool, aiming to reduce referrals into secondary care. Whilst it is accepted that A&G is a useful tool to reduce referrals to secondary care of patients who could be equally well managed in primary or community care settings, there is significant concern in our survey that the responses from secondary care were sometimes asking for unrealistic investigations to be performed by primary care, many of which are not available in the community, and would ordinarily have been requested within secondary care, at or prior to the outpatient appointment post referral. In addition, there were increasing numbers of referrals being rejected and converted to A&G offering advice on management within the community, rather than seeing the patient in secondary care.
Is A&G being used to reduce referrals in your area?
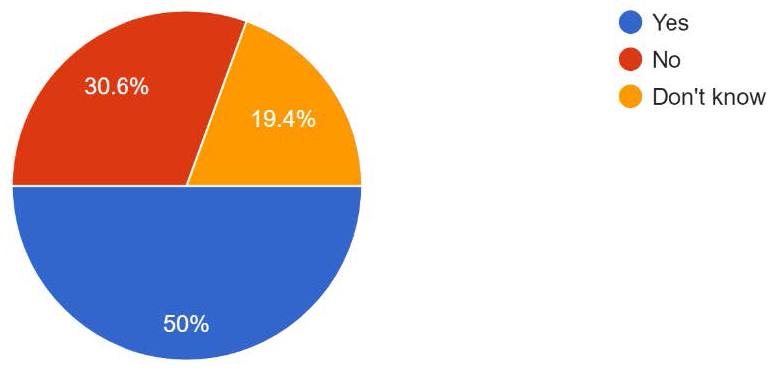
There is variability across the system in terms of the impact on GP workload. 50% of respondents believed A&G increased workload within primary care, because it was used as a way to move the initiation of investigations and treatment into primary care that would ordinarily be commenced in secondary care. This led to some respondents describing having to treat conditions that they felt outside of their clinical competence based on A&G responses.
Whilst NHS Digital states the aim of the service since the changes in February 2021, are to “reduce the burden on GPs/referrers”, by allowing “advice and guidance to be used as a referral channel”, our survey has found in some areas the opposite is happening. A&G is being used by some providers to hold a conversation between clinicians, rather than accepting the referral requested by primary care. It was noted that this then increases the workload within general practice as for every A&G response, the primary care team needs to book a further patient appointment, and if further questions are raised, create another A&G request. The concern is that this may lead to delays in diagnosis, treatment, and increased numbers of primary care consultations when referrals are rejected and then converted to A&G instead.
30% of respondents, however, did not believe it increased workload instead finding the service useful in streamlining patient care, improving access to expert advice and improving knowledge of primary care teams.
Does' Advice and Guidance' increase your workload?
If a patient is referred to secondary care, the clinical risk is then held by secondary care. If a referral is declined, in favour of A&G, then clarification of where the clinical risk lies is required. The RCGP believes the clinical risk should be shared between the clinicians in primary and secondary care and not lie solely in primary care.
In some areas of the country, there are IT issues meaning GPs must log into the secondary care system to continually check for A&G responses, increasing the administrative burden on practices. This is not universal.
Some GPs commented that there was no identifiable clinician on their A&G responses and so if further questions arose, there was no consistent clinical contact available. This also makes it difficult to trust the advice being given, without understanding the level of the advisers. It is essential that any clinical decision made in primary or secondary care follows GMC guidance on good record keeping, identifying the person who gave the advice or made the clinical decision.
- Further support for collaboration between primary and secondary care is essential to enable the backlog of care exacerbated as a result of the pandemic to be managed and streamline patient care.
- If work is to be transferred from secondary to primary care, via A&G, then resource (time, money and people) must follow the patient and not stay in secondary care.
- A&G should be optional and not mandated.
- Other tools to promote closer working between primary and secondary care aiming to streamline patient care are available and should be considered by providers as alternatives, allowing choice. These include direct telephone calls, emails, teledermatology and commercial apps that are able to connect primary and secondary care.
- Clinical care governance and risk must be shared between primary and secondary care during A&G conversations, and this must be understood by all clinicians and their patients when A&G is used.
- When using A&G, all clinicians must uphold the standards of good medical record keeping as per GMC advice, documenting decisions and actions, identifying who has made the decisions and is agreeing with the actions, in the patient clinical record. This should apply to both primary and secondary care and not rely solely on primary care updating the clinical records.
Thank you for your feedback. Your response will help improve this page.