Thank you for your feedback. Your response will help improve this page.
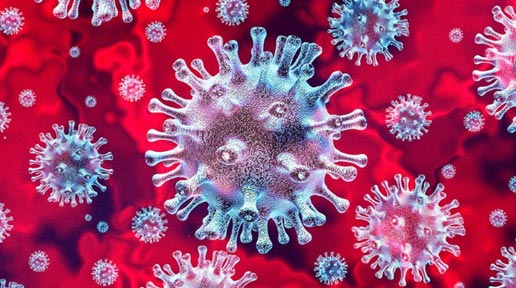
The COVID-19 outbreak is arguably one of the greatest public health challenges of our time - not least for general practice, where over 1 million patients are already treated every day.
Thank you for your feedback. Your response will help improve this page.
Some of these cookies are essential, while others help us to improve your experience by providing insights into how the site is being used. By clicking accept you agree to analytical and marketing cookies. You can opt out by clicking reject or by using the individual controls below.
Read more about our Cookie Policy in our Privacy policy.
Necessary cookies enable core functionality such as page navigation and access to secure areas. The website cannot function properly without these cookies, and can only be disabled by changing your browser preferences.
We use software including Google Analytics to help us improve our website by collecting and reporting information on how you use it. The cookies collect information in a way that does not directly identify anyone.
These cookies are used to show you ads that are relevant to you, limit the number of times you see them, and measure their performance. They are usually placed by third parties, such as advertising networks, with our permission.